That means media-makers (reporters, editors, radio and TV hosts, bloggers, TV personalities, public relations professionals, etc.) have a responsibility to use care and professionalism when covering topics related to HIV and/or people living with HIV. Using people-first language and taking every available opportunity to share up-to-date, accurate information about HIV treatment, prevention, and actual transmission risks is critical. So is being sure to treat disclosure as the complicated issue that it is. This page will provide you with guidelines and resources for covering HIV in the media.
The stigma attached to HIV is a significant barrier to living well with HIV. By working together, we can raise awareness and help improve the lives of those living with HIV by being mindful of our language. Language can be a tool to empower, or to further stigmatize.
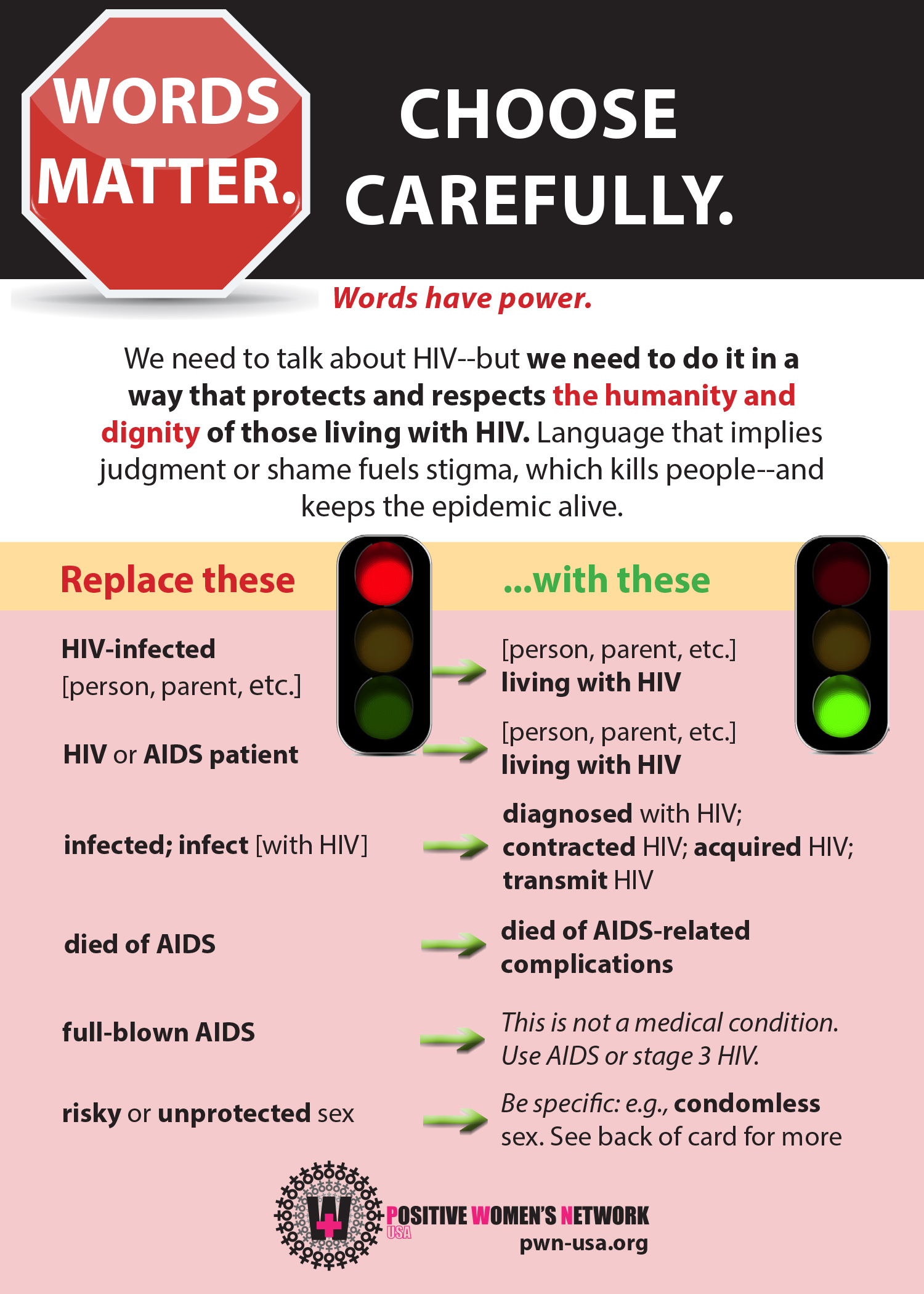
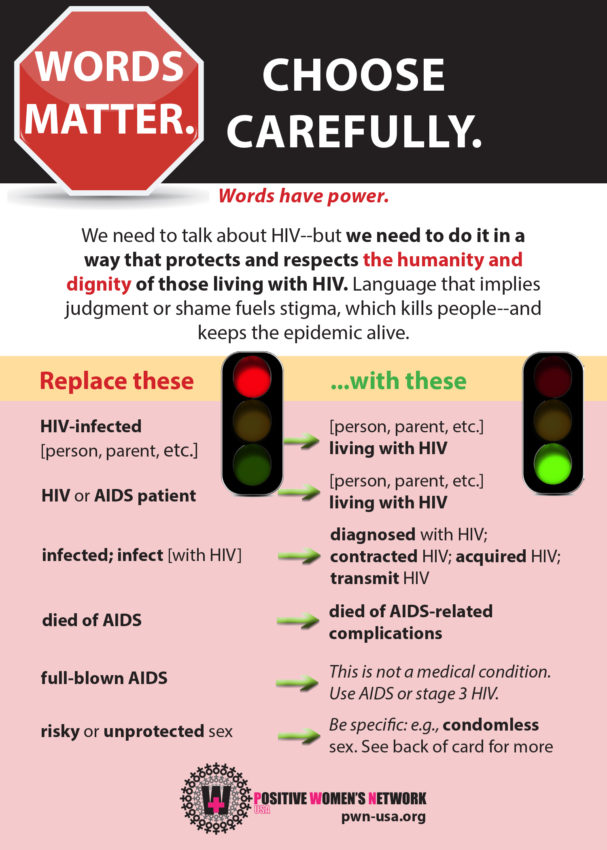
| Replace These Stigmatizing Terms… | …with These Preferred Terms! |
|---|---|
| HIV-infected person HIV-positive person HIV carrier HIV (or AIDS) patient |
Person (parent, etc.) living with HIV |
| Infected with HIV | Diagnosed with HIV; contracted HIV; acquired HIV |
| Catch AIDS | Develop an AIDS diagnosis; develop AIDS (contract HIV) |
| AIDS virus | HIV (AIDS is a diagnosis, not a virus; it cannot be transmitted) |
| Infect with HIV | Transmit HIV |
| Die of AIDS | Die of AIDS-related illnesses or complications; die of end stage HIV |
| HIV virus | HIV (this is redundant; the word virus is already in the term HIV) |
| Full-blown AIDS | AIDS; stage 3 HIV (“full-blown AIDS” is not a medical term and does not mean anything) |
| Clean/dirty | Do not use |
| Risky or unprotected sex | Be specific–e.g., condomless sex |
| Victim; sufferer; contaminated | Do not use |
| AIDS orphan | Child orphaned by the loss of parents due to complications of AIDS |
| Mother to child transmission | Vertical transmission; perinatal transmission |
| Bodily fluids | Be precise on which fluids you are referring to blood, semen, vaginal fluids or secretions, breast milk, amniotic fluid, pre-ejaculate. (Some fluids, like urine and saliva, do not carry or transmit HIV) |
| Injection drug user; drug addict | Person who injects drugs or person who uses drugs |
| Prostitute; prostitution | Person who does sex work, sex worker, participates in street economy or transactional sex work |
| Promiscuous | Having multiple partners (promiscuous is a value judgment and should be avoided) |
| Fight against AIDS; fight to end HIV | HIV response; fight to end HIV transmission |
| Compliant | Adherent; taking medications as prescribed |
As often as not, those of us who are people living with HIV are framed in media as monsters, infected, dirty, predatory, and more. Those who are reported as having acquired HIV – or having been intimate with a person with HIV – are labeled as victims or as having been preyed upon. In truth, people living with HIV are just that: people.
HIV is the human immunodeficiency virus that attacks the CD4 cells within a PERSON. And many of our partners choose to be with us because they love us and it is not “risky” to be intimate with us.
Furthermore, science has proven in recent years, through numerous large-scale, long-term studies looking at thousands of serodifferent couples and hundreds of thousands of condomless sex acts, that a person who achieves an undetectable viral load through effective treatment cannot transmit HIV to their sexual partners–even without condoms. (See the next toggle for more information.)
Therefore:
- Coverage of people living with HIV should highlight accomplishments and achievements that are not focused on the virus.
- Stories of people living with HIV should include our strength, survival, and courage.
- The media could promote the importance of ending stigma, to create environments safe for knowing one’s status, HIV testing, and open communication with partners.
HIV transmission is not possible, under any circumstances, through a hug, a handshake, a toilet seat, sharing a cup, or eating food cooked by a person with HIV. Period. The fact that these myths persist in the general population is damaging to the wellbeing of people with HIV, and shows how great the need is for reporting on HIV that is not only accurate, but that actively counters misinformation.
2. Undetectable=Untransmittable. When a person living with HIV takes their antiretroviral medications as prescribed–often just one pill a day–they can reduce the amount of virus in their body to levels that are not detectable in labs. This is called an “undetectable viral load,” and it allows people living with HIV to stay healthy and live a normal life span.
In recent years, numerous large-scale, long-term studies (including HPTN 052, PARTNER, and PARTNER 2), that studied thousands of serodifferent couples (where one partner has HIV and the other does not) and hundreds of thousands of condomless sex acts, have confirmed that a person living with HIV with an undetectable viral load cannot transmit HIV to their sexual partners, even without condoms. This is called undetectable=untransmittable, or U=U.
It is important to share this information whenever reporting on HIV.
It is also important to recognize and remember that there are many barriers to people living with HIV reaching undetectable, including lack of access to affordable health care; stigma and bias among medical providers; and lack of supportive services that help people get and remain in care (e.g., housing, mental health care, substance abuse treatment, transportation, etc.), among others. People deserve to be treated with respect and dignity, regardless of whether or not they have reached an undetectable viral load.
Read more about that excellent and no-longer-new news here and here.
4. Laws that criminalize HIV-positive status do not protect or help women. As of this writing, 35 states have HIV-specific laws that attach criminal penalties to the behavior and actions of people living with HIV. These laws are often framed in the media as protecting women “victims” from dishonest partners, but the laws help no one.
These laws codify stigma, and actually deter people from getting tested or being in care (a person who doesn’t know their HIV status cannot be prosecuted for HIV nondisclosure or exposure), thereby hindering public health solutions. That is why CDC and Department of Justice employees who studied the public health consequences of HIV criminalization have encouraged states to review and update their HIV criminalization laws, and why 20 global scientific experts in HIV signed a consensus statement in 2018 that HIV criminalization should end.
In most HIV-related prosecutions, no transmission of HIV even occurred! Further, women have been sent to prison under these laws, and/or had their children taken away for no reason – often by partners who knew the woman’s HIV status but used the laws as a tool of abuse, coercion, or harassment when the woman attempted to end the relationship. Making it a crime not to disclose HIV-positive status should never be framed as the answer to addressing HIV in communities or to keeping people HIV negative.
HIV is not just a man’s issue; it never has been. Talk to women living with HIV.
If you are not engaged in conversations about HIV with women of color, you are really missing the point. You may be missing the whole truth, the undisputed truth, the unadulterated story of HIV in the U.S.
PWN has a number of official member spokespeople you can contact who can speak to the issues they and other women living with HIV face. You can find contacts here, or get in touch with our communications team at communications(at)pwn-usa.org.
- Positive Women’s Network – USA (PWN-USA) – Features a wide variety of advocacy resources for women with HIV, including opinion pieces and statements highlighting the perspectives and expertise of women advocates living with HIV.
- International Community of Women Living with HIV (ICW) – The only global network by and for women with HIV; features stories of women living with HIV around the world.
- The Well Project – Features cutting-edge information, personal reflections, and research by and for women with HIV.
- TheBody.com’s Women’s Resource Center – Features first-person stories and videos by women living with HIV, as well as basic information about women and HIV.
A person’s choice to tell someone their HIV status is complicated. Write about HIV disclosure as the complicated issue it is.
Further, in the presence of laws that penalize people with HIV for knowing their HIV status, disclosing won’t protect a woman in a he-said-she-said argument in court, where the person who knows their HIV-positive status usually loses. Women are often the first person in the relationship to be aware of their HIV-positive status.
One answer to empowering individuals in their relationships and fostering healthy, safe communication is to address the root causes of inequities that impact our lives and relationships, and drive the HIV epidemic – and to ensure comprehensive, medically accurate sex education. The solutions is not to blame people for having HIV, or cast their sexual partners as “victims.” Where there is a victim, there must be a perpetrator, and having HIV is not a crime.
Any trait that sets a person apart from a societal norm can be challenging to talk about, or to disclose. HIV status is no different.
When journalists convey messages that shame the sexuality of people with HIV in their reporting – as if to even be having sex as a person with HIV is somehow wrong – or imply that finding love, having sex, or being in relationships is impossible for people living with HIV, they validate that assumption. A healthy dose of nonjudgmental, sex-positive messaging in mainstream media could save and improve lives.
Resources for Media-Makers
Reporting with Care: Updating How We Talk About HIV in the Media
Eliminating Stigma from the Language of HIV Communications
Special thanks and deep gratitude to all the insightful PWN members who acted as co-authors and contributors to this statement:
Valerie Wojciechowicz · Venita Ray · Naimah Oneal · Susan Mull · Asha Molock · Vickie Lynn · Tiommi Luckett · Vanessa Johnson · Olga Irwin · Tami Haught · Barb Cardell